INDICATIONS
Gastrojejunostomy is indicated for certain elderly patients with duodenal ulcer complicated by pyloric obstruction and low acid value. It is indicated also if technical difficulties prevent resection or make it hazardous, if the patient is such a poor operative risk that only the safest possible surgical procedure should be carried out, or if vagus resection has been performed. It is occasionally indicated for the relief of pyloric obstruction in the presence of nonresectable malignancies of the stomach, duodenum, or head of the pancreas. Gastrin levels should be determined.
PREOPERATIVE PREPARATION
The preoperative preparation must be varied, depending upon the duration and severity of the pyloric obstruction, the degree of secondary anemia, and the protein depletion. The restoration of blood volume is especially important in patients who have lost considerable weight. Low values of sodium chloride and potassium must be corrected, and the carbon dioxide combining power and blood urea nitrogen returned to normal before operation. Secondary anemia and protein and vitamin deficiencies should be corrected insofar as possible before operation. Their correction aids healing and contributes to the proper emptying of the stomach after operation. The large atonic stomach is emptied by constant gastric suction for several days before operation. The stomach is emptied by gastric lavage, usually the night preceding operation, to make certain that all coarse particles of food have been removed and that gastric tension is relieved. The lavage is repeated one to two hours before operation. Constant gastric suction with a Levin tube is maintained. Blood must be available for transfusion during the operation.
ANESTHESIA
General anesthesia combined with endotracheal intubation is usually satisfactory. Muscle relaxants may be employed to avoid the deeper planes of anesthesia. Spinal or continuous spinal anesthesia provides profound muscle relaxation and a contracted bowel. Local infiltration is sometimes advisable in poor-risk patients.
POSITION
The patient is placed in a comfortable supine position with the feet at least a foot lower than the head. In patients with an unusually high stomach, a more upright position may be of assistance. The optimum position can be obtained after the abdomen is opened and the exact location of the stomach is determined.
OPERATIVE PREPARATION
The lower thorax and abdomen are prepared in the routine manner.
INCISION AND EXPOSURE
As a rule, midline epigastric incision is made. The incision is extended upward to the xiphoid or to the costal margin and downward to the umbilicus. With the abdomen opened, a self-retaining retractor may be utilized; but since most of the structures involved in this operation are mobile, it is usually unnecessary to use any great amount of traction for adequate exposure.
DETAILS OF PROCEDURE
The stomach and duodenum are visualized and palpated to determine the type and extent of the pathologic lesion present. A short loop of jejunum is utilized for gastrojejunostomy, with the proximal portion anchored to the lesser curvature. The stoma is made on the posterior gastric wall and extends from the lesser to the greater curvature, about two fingers in length. It is located at the most dependent part of the stomach (Figure 1, A).
When the gastroenterostomy is performed with vagotomy in the treatment of duodenal ulcer, the location and size of the stoma are very important. In order to ensure adequate drainage of the paralyzed antrum and keep postoperative side effects to a minimum, a small stoma parallel to the greater curvature and near the pylorus is indicated (Figure 1, B). The jejunum should be anchored for several centimeters to the gastric wall on either side of the stoma. This permits circular uncut muscles going away from the stoma to contract and improve gastric emptying. Special effort is required as a rule to ensure placement of the stoma within 3 to 5 cm of the pylorus. Because of the fixation of the pylorus associated with duodenal ulceration, it is too impractical to attempt to bring the site of the anastomosis outside the abdominal wall, as shown in the accompanying diagrams.
The location of the stoma is first outlined on the anterior gastric wall with Babcock forceps. The greater omentum may be brought outside the wound so that the contour of the stomach is not distorted, and the most dependent portion of the greater curvature may be more accurately determined (Figure 2). The Babcock forceps are left in place as the greater omentum is reflected upward over the stomach and the inferior aspect of the mesocolon is visualized (Figure 3). The transverse colon is held firmly by an assistant as the surgeon invaginates the Babcock forceps on the anterior gastric wall. This produces a bulge in the mesentery of the colon at the point through which the stomach is to be drawn (Figure 3). The mesocolon iscarefully incised to the left of the middle colic vessels and near the ligament of Treitz, great care being taken to avoid any of the large vessels in the arcade. Four to six guide sutures (sutures a, b, c, d, e, and f) are placed in the margins of the incised mesocolon to be utilized after the anastomosis to the stomach at the proper level. The presenting posterior wall of the stomach is grasped with a Babcock forceps adjacent to the lesser and greater curvatures, and opposite the points of counterpressure from the similarly placed forceps on the anterior gastric wall (Figure 4). A portion of the gastric wall is pulled through the opening. In many instances the inflammatory reaction associated with the duodenal ulcer may anchor the posterior surface of the antrum to the capsule of the pancreas. Sharp and blunt dissection may be required to mobilize the stomach in order to ensure placement of the stoma sufficiently near the pylorus. Some surgeons prefer to anchor the mesocolon to the stomach at this time. The forceps on the greater curvature is swung toward the operator on the patient's right side, while the forceps on the lesser curvature is rotated to a position opposite the first assistant.
The ligament of Treitz is identified, and a loop of jejunum 10 to 15 cm distal to this fixed point is delivered into the wound. The jejunum at this point is held with Babcock forceps as the enterostomy clamp is applied. The midsection of the portion of jejunum to be included in the enterostomy clamp may require fixation with thumb forceps to assure an even inclusion of the bowel in the clamp (Figure 5). The clamp should be applied near the mesenteric border, with the handle of the clamp toward the patient's right side and with the proximal jejunal loop in the toe end of the clamp (Figure 5).
Spring clamps are best used without rubber covers, because covers make them bulky and so slippery that more pressure is likely to be used than is necessary, especially at either end of the clamp. A clamp of fine spring steel holds its position well without great pressure and leaves no deleterious effects.
With the clamp in position, a piece of gauze is laid next to the jejunum. Then the stomach is grasped in a similar enterostomy clamp, placed with the handle of the clamp toward the patient's head, to include the selected oblique portion of the posterior gastric wall (Figure 6). Now the two enterostomy clamps are bought side to side, so that the distal end of the jejunal opening will be at the greater curvature of the stomach. The portion of the jejunum toward the ligament of Treitz, i.e., the proximal portion, is anchored to the lesser curvature of the stomach (Figure 6). At times the stomach cannot be sufficiently mobilized for the application of clamps as shown in Figure 6, and the anastomosis is made without a clamp on either side.
The enterostomy clamps applied to the stomach and the jejunum are held in apposition by ligatures or rubber bands (Figure 7, x and y). The large intestine and omentum are returned within the abdomen above the stomach. The clamps and the anastomotic site usually can be delivered outside the peritoneal cavity, which should be entirely protected with gauze. Retraction on the edges of the abdominal wound is discontinued while the anastomosis is being performed. This mobilization is usually impossible when the stoma must be made within 3 to 5 cm of the pylorus following vagotomy. Under these circumstances the anastomosis must be made within the peritoneal cavity, lest the stoma be made too far to the left, with recurrent ulcer difficulties due to hormone stimulation from the distended antrum inducing gastric hypersecretion.
The posterior serosal sutures are now begun by placing a mattress suture of fine silk at either angle (Figure 7). The surgeon depresses the presenting portions of the stomach and jejunum with his index and middle fingers as the posterior row of interrupted mattress sutures in the serosa, parallel with the enterostomy clamp, is completed (Figure 8). Alternate bites of jejunum and stomach are taken; these include the submucosa but do not enter the lumen of the bowel. Each suture is taken close to the preceding one to ensure a complete closure. It is best to tie them after all have been placed.
When the posterior serosal layer is completed, fresh moist toweling is laid on both sides of the field; the only instruments left on this toweling are those to be used for opening the stomach and jejunum, for cleaning the lumen, and for closing the bowel with the mucosal sutures.
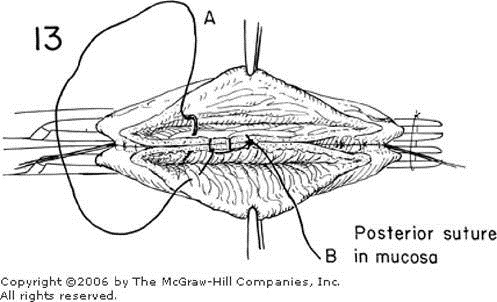
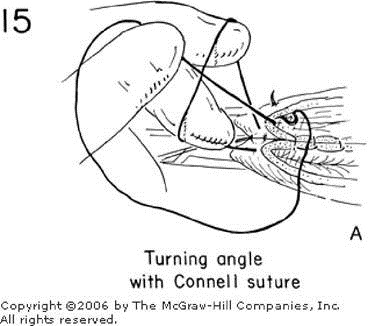
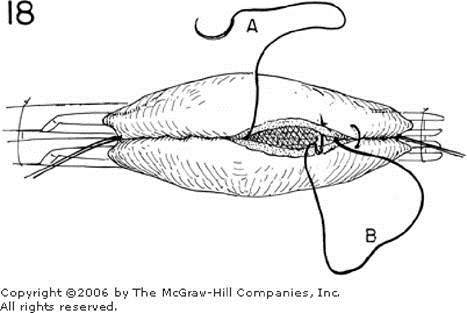
Short, lengthwise incisions in the stomach and jejunum are made by depressing the bowel and incising the a scalpel several millimeters from the serosal suture and not in the middle of the presenting contents of the clamp (Figure 9). If this incision is too far from the serosal layer, too large a cuff of inverted bowel may result. In making these incisions, the operator should be careful to cut the bowel wall perpendicular to its surface, since there is always a tendency to incise the intestine obliquely, thereby leaving an irregular and unequalized mucosal layer for the next suture line (Figure 10). The larger vessels in the stomach wall are then ligated with 0000 transfixing sutures of silk. The contents of the bowel are wiped out with a small piece of gauze moistened with saline, and the mucosal incision is completed with straight scissors. The incision in the jejunum is made slightly shorter than that made in the stomach (Figure 11). With the stomach and intestine opened and cleaned, a continuous absorbable suture on straight needles is started in the midportion of the posterior mucosal layers (Figure 12). Although straight needles are shown, absorbable sutures swedged on curved needles are most commonly used. As the operator sews away from himself or herself, he or she uses a simple over-and-over suture or a lock stitch, which pulls together the mucosal layers (Figure 13). Since this suture is also used to control the blood supply, it must be kept under a tension sufficient for accurate approximation and prevention of hemorrhage, yet not completely strangulating the blood supply and hindering healing. This is a critical step. The amount of tension is adjusted by the surgeon, who should hold the suture in his or her left hand while he or she works with the right. The first assistant exposes the point to be sutured and pulls the needle through. Interrupted sutures are placed to secure any bleeding points that have not been controlled by the continuous suture. When the operator reaches the angle of the wound, a Connell suture, which allows inversion of the structures as they are sewn, is substituted (Figure 14). In Figure 14, for example, the needle has just entered the gastric side. It comes out on the gastric side 2 or 3 mm from its point of entrance (Figure 15). It is then crossed over, inserted through the jejunal wall from outside as in Figure 16, and comes back out through the jejunal wall before being reinserted through the gastric wall (Figure 17). After this angle has been closed, the other end, B, of the continuous suture is used to close the opposite angle in a similar fashion (Figure 18). The continuous sutures, A and B, finally meet along the anterior surface. The final bite of each suture brings it to the inner wall of the stomach and jejunum (Figure 19). The two ends are tied together with the final knot on the inside. The clamps may then be released to see whether there is any bleeding. If slight oozing persists, additional interrupted sutures may be taken to supplement the anterior mucosal layer.
Some surgeons prefer to do the anastomosis without clamps and tie each individual bleeding point before approximating the mucosa. Others prefer interrupted fine 0000 silk sutures for the mucosa instead of a continuous suture. The interrupted sutures on the anterior surface are tied with the knot on the inside. This series of interrupted Connell-type sutures ensures an even inversion of the mucosa.
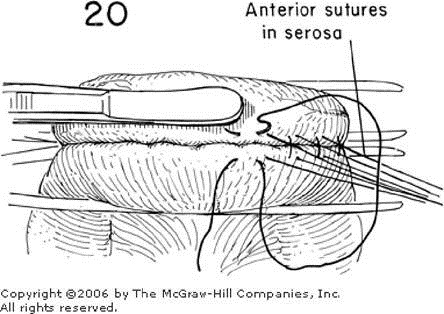
The special toweling and the instruments used for the preceding stage of the operation are discarded; the gloves are changed, or gloved hands are thoroughly washed in an antiseptic solution, and approximation of the anterior serosal layer is carried out with interrupted fine silk sutures (Figure 20). These are placed very close together. Additional interrupted sutures of fine silk are placed at the angles of the anastomosis for reinforcement so that any strain at this point avoids the original suture line (Figure 21). The patency and size of the stoma should be determined by palpation. A secure anastomosis is desirable with a stoma approximately the size of the end of the thumb or two fingers.
A stoma about one half the size illustrated is indicated when vagotomy is performed. The lumen should not be larger in diameter than the adult thumb in order to reduce the incidence and severity of postoperative complaints. The stomach is anchored to the mesocolon, with sutures b, c, and d (Figure 21) adjacent to the anastomosis in order to close the opening and thus prevent a potential internal hernia. This also prevents any torsion of the jejunum near the anastomosis, which might result if the stoma retracts above the mesocolon (Figure 22).
Occasionally, in the presence of extensive inflammation about the pylorus, marked obesity, or extensive malignancy, it may be impossible to mobilize the posterior gastric wall sufficiently for an anastomosis that allows adequate drainage of the antrum. Under these circumstances anterior gastrostomy or enterostomy should be considered following vagotomy to ensure adequate drainage of the antrum or proximal drainage of an inoperable gastric malignancy. In order to avoid the possibility of poor emptying following anterior gastrojejunostomy, the thick omentum should be divided to permit the upper jejunum to be easily brought up over the transverse colon. Some prefer to clear the greater curvature near the pylorus for 5 to 8 cm and place the gastrojejunal stoma in this area. The antecolic efferent jejunal loop should be anchored to the anterior gastric wall for approximately 3 cm beyond the anastomosis to provide uncut circular muscle contractions to assist in gastric emptying. A Stamm-type gastrostomy should be considered to ensure patient comfort and provide an efficient and readily available method of gastric decompression until gastric emptying is satisfactory.
CLOSURE
The wound is closed in the routine manner. It is not drained.
POSTOPERATIVE CARE
Constant gastric suction is maintained for several days until it is evident that the stomach is emptying satisfactorily. The use of fluids, glucose, vitamins, and parenteral alimentation depends upon daily clinical and laboratory evaluation. The patient may be permitted out of bed on the first day after operation. Water in sips is given within 24 hours, and the fluid and food intake is increased gradually thereafter. Six small feedings per day are gradually replaced by a full diet as tolerated. Gastric secretion studies should be done to evaluate the completeness of the vagotomy when the latter procedure has been performed in the treatment of duodenal ulcer. If a gastrostomy has been done, the tube can usually be withdrawn in 10 days unless there is evidence of a delay in gastric emptying.
Copyright ©2006 The McGraw-Hill Companies. All rights reserved. Privacy Notice. Any use is subject to the Terms of Use and Notice. Additional Credits and Copyright Information.