INDICATIONS
The usual indications for gastrostomy include the need for feeding, decompression, or gastric access. In feeding situations, the gastrointestinal tract must be functional and the need for enteral feeding must be for a prolonged interval. Stamm gastrostomies are most commonly performed at the conclusion of some other major gastrointestinal procedure while the abdomen is open, whereas historically the need for a gastrostomy necessitated only a laparotomy with general or local anesthesia. The percutaneous endoscopic gastrostomy (PEG) allows the placement of a gastrostomy in adults and children without laparotomy. This technique depends upon the safe passage of an endoscope into the stomach, which can be dilated with air. Inability to pass the endoscope safely or inability to identify the transabdominal lumination of the lighted endoscope tip within the dilated stomach are contraindications to the procedure. Ascites, partially corrected coagulopathy, and intra-abdominal infection are relative contraindications to the PEG method.
PREOPERATIVE PREPARATION
The indications for the gastrostomy dictate the extent and type of preoperative preparation. Passage of a nasogastric tube for gastric decompression is usually not needed if the patient has been NPO for several hours. A single dose of intravenous antibiotic is given immediately prior to the procedure because the peroral passage of the special catheter may contaminate the abdominal wall tract created as the catheter is brought out through the stomach.
ANESTHESIA
A topical anesthesia for the oropharynx is needed for passage of the endoscope, and local anesthesia is used at the abdominal site where the special catheter will be placed. An intravenous needle or catheter is positioned for administration of sedatives.
POSITION
The patient is usually supine while the topical anesthetic is sprayed into the oropharynx. He or she is allowed to gargle, swallow, or spit into a basin. After satisfactory anesthesia is obtained, the patient is positioned supine on the table with the head slightly elevated.
OPERATIVE PREPARATION
In adults as well as children, the smallest possible gastroscope is used. After the endoscope is passed safely into the stomach, the skin of the abdomen and lower chest is prepared with antiseptic solutions in the usual manner. Sterile drapes are applied.
DETAILS OF PROCEDURE
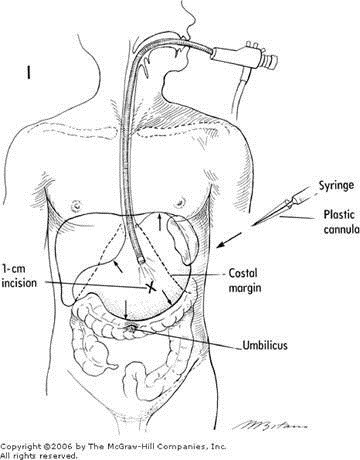
During the placement of the gastroscope, any pathology may be evaluated. The stomach is fully inflated with air. This displaces the colon inferiorly and places the anterior gastric wall against the abdominal wall over a large area. A suitable zone is selected and the endoscopist places the lighted gastroscope end firmly upwards at this point. This is usually halfway between the costal margin and the umbilicus (Figure 1). The operating room lights are dimmed and the transilluminated site is identified. In very thin patients, the tip of the endoscope may be palpated. The area of transillumination is marked (Figure 1, X). The endoscope is backed away from the anterior gastric wall, and the appropriateness of the site is verified as external palpation with a finger indents the chosen area.
Local anesthesia is injected and a 1-cm skin incision is made. The endoscopist visualizes the site as a 16-gauge smoothly tapered intravenous cannula/needle is introduced through the incision, abdominal, and gastric walls and into the lumen of the stomach. This sequence should be done quickly so as to minimize the chance for displacement of the stomach away from the abdominal wall and peritoneum.
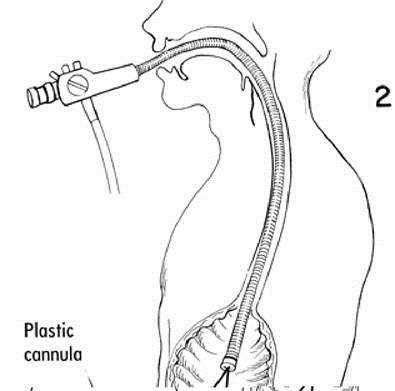
A long large silk or nylon suture is passed through the hollow outer cannula after the stiffening inner needle has been withdrawn. The silk is grasped with a polypectomy snare passed through the endoscope and then all are withdrawn through the patient's mouth (Figure 2). A dePezzer catheter (Figure 5) with the inner crosspiece (a cut section of tubing) or a special PEG catheter (Figure 3) is secured to the long suture. The catheter must have a tapered end; if necessary, one is created with a tapered plastic cannula that will enclose the open end of the dePezzer catheter. The long suture and the catheter assembly are covered with a sterile water-soluble lubricant. Gentle, steady traction on the abdominal end of the long suture pulls the tapered end of the assembly down the esophagus and then through the gastric and abdominal wall (Figure 4).
The endoscope is reintroduced and the positioning of the special catheter of crosspiece is verified. An external crosspiece (Figure 5) or collar is applied, and a nonabsorbable suture is used to secure the catheter and crosspiece to the skin without pressure or tension that might necrose the skin. The small skin incision is left open and topical antiseptic may be applied.
POSTOPERATIVE CARE
The gastrostomy catheter is opened for decompression and gravity drainage for a day. Thereafter feedings may start in a sequential manner beginning with small, dilute volumes. The catheter may be changed in a periodic manner or may be converted to a silastic prosthesis after four weeks or more when the gastrostomy incision has solidly healed and the stomach has fused to the anterior abdominal wall. This prosthesis is stretched and thinned over an obturator (Figure 6) and inserted into the open gastrostomy tract (Figure 7).
Copyright ©2006 The McGraw-Hill Companies. All rights reserved. Privacy Notice. Any use is subject to the Terms of Use and Notice. Additional Credits and Copyright Information.