INDICATIONS
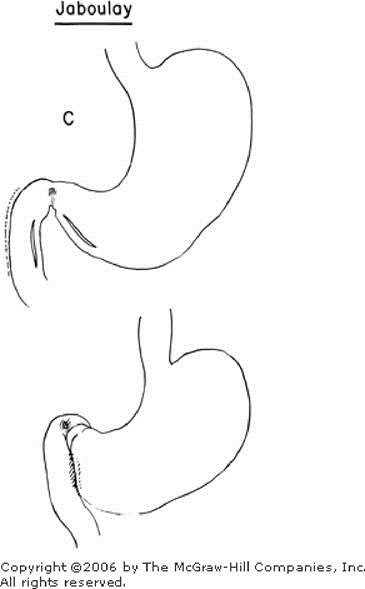
These procedures may be used when the vagus innervation of the stomach has been interrupted either by truncal vagotomy, selective vagotomy, or division of the vagus nerves associated with esophagogastric resection and reestablishment of esophagogastric continuity. The pyloroplasty ensures drainage of the gastric antrum following vagotomy and therefore partially eliminates the antral phase of gastric secretion. It does not alter the continuity of the gastrointestinal tract and decreases the possibility of marginal ulceration occasionally seen after gastrojejunostomy. Pyloroplasty carries a low surgical morbidity and mortality rate because of its technical simplicity. Two types of pyloroplasty are commonly used: the Heineke-Mikulicz pyloroplasty (Figure A) and the Finney pyloroplasty (Figure B). Pyloroplasty should be avoided in the presence of a marked inflammatory reaction or severe scarring and deformity on the duodenal side of the gastric outlet. Under these circumstances the Jaboulay procedure (Figure C) should be considered, or a gastroenterostomy located within 3 cm of the pylorus on the greater curvature. Gastrin levels should be determined. The Jaboulay reconstruction should be considered when a long incision is made in the anterior wall of the duodenum during the search for very small mucosal gastrinomas.
Heineke-Mikulicz Pyloroplasty (Figure A)
The pylorus is identified with the pyloric vein as the landmark. A Kocher maneuver (see Gastrectomy, Subtotal, Figures 1, 2, 3, 4, 5, 6, and 7) is then carried out to mobilize the duodenum for good exposure and relaxation of tension on the subsequent transverse suture line. Traction sutures of 00 silk are placed and tied at the superior and inferior margins of the pyloric ring for anatomic orientation. Efforts should be made to include the pyloric vein in these sutures, inorder to partially control the subsequent bleeding. A longitudinal incision is made approximately 2 to 3 cm on each side of the pyloric ring through all layers of the anterior wall (Figure 1). In the presence of marked deformity it may be advisable to incise the midportion of the duodenum and then, with a hemostat directed up through the constricted pyloric canal as a guide, make the incision in the midportion of the pylorus, across the midportion of the anterior duodenal wall, and across the midpoint of the pyloric wall into the gastric side. Bleeding may be partially controlled by noncrushing clamps across the antrum and distal to the anastomosis across the duodenum, unless the induration and fixation associated with the ulcer are too marked.
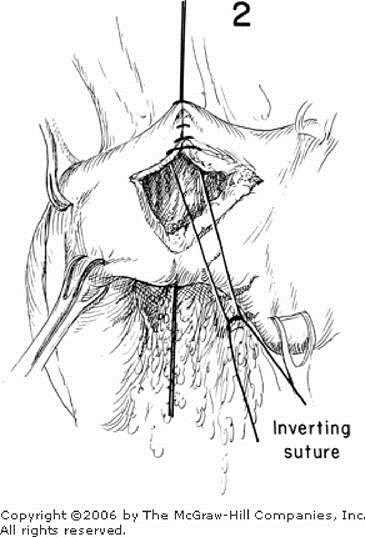
Traction on the angle sutures draws the longitudinal incision apart until it becomes first diamond shaped (Figure 1) and then transverse (Figure 2). All bleeding points are ligated with 0000 silk which includes the full thickness of gastric or duodenal wall. Active bleeders tend to occur in the divided duodenal wall and in the region of the divided pyloric sphincter. Inverting sutures of interrupted 0000 silk are passed through all layers to approximate the mucosa. Some prefer a one-layer closure (Figure 2) in order to minimize the encroachment on the pyloric lumen resulting from the inversion that follows a two-layer closure. The one layer, Gambi suture, is shown in cross section. This placed in four passes, with the second and third bites involving only the gastric or duodenal mucosa (Figure 3). The result is complete inversion with good serosa-to-serosa approximation. After the closure is completed, the thumb and index finger are used to palpate the newly formed lumen by invaginating the gastric and duodenal walls on each side of the transverse closure. A Cushing silver clip may be placed to mark either end of the suture line to serve as a marker of the gastric outlet during subsequent barium studies. A temporary gastrostomy may be performed (see Gastrostomy).
Finney U-Shaped Pyloroplasty (Figure B)
The pylorus is identified by noting the overlying pyloric vein. Freeing all interfering adhesions and mobilizing the pyloric end of the stomach, the pylorus, and the first and second portions of the duodenum by use of an extensive Kocher maneuver are essential (see Gastrectomy, Subtotal, Figures 1, 2, 3, 4, 5, 6, and 7). A traction suture is placed in the superior margin of the midpylorus, and a second suture joins a point approximately 5 cm proximal to the pyloric ring on the greater curvature of the stomach to a point 5 cm distal to the pyloric ring on the duodenal wall (Figure B). The walls of the stomach and duodenum are sutured together with interrupted 00 silk. These sutures should be placed as near the greater curvature margins of the stomach and the inner margin of the duodenum as possible, to ensure adequate room for subsequent closure. A U-shaped incision is then made into the stomach from a point just above the traction suture, around through the pylorus, and down a similar distance on the duodenal wall adjacent to the suture line. If an ulcer is present on the anterior wall, it may be excised. Bleeding points are clamped and tied with 0000 silk. A wedge of the pyloric sphincter may be removed from either side to facilitate the mucosal closure. The posterior mucosal septum between the stomach and duodenum is united with interrupted 0000 silk sutures. These sutures run from the superior aspect and include all layers of the septum (Figure 4). The anterior mucosal layer is approximated with inverting interrupted sutures of 0000 silk.
As seen in Figure 5, a second layer of sutures using a mattress overlapping stitch starts superiorly and brings together the seromuscular layers of the anterior walls of the stomach and duodenum. A portion of the omentum may be sutured over the anastomosis. A temporary gastrostomy may be performed (see Gastrostomy) or constant nasogastric suction maintained a few days or until the stomach empties satisfactorily.
Jaboulay Gastroduodenostomy (Figure C)
It is advisable to carry out a very extensive Kocher maneuver (see Gastrectomy, Subtotal, Figures 1, 2, 3, 4, 5, 6, and 7) with through mobilization of the second and third parts of the duodenum. When this procedure is carried out, it is wise to visualize the middle colic vessels, which sometimes tend to swing down over the duodenum and appear rather unexpectedly during the dissection. It is also advisable to attempt a limited mobilization of the inner surface of the duodenum without interference with its blood supply. The gastric wall, however, adjacent to the pylorus and downward for 6 to 8 cm may be freed of its blood supply and tested for mobility over to the duodenal wall. A suture is taken between the gastric wall and duodenum as near the pylorus as practical, and a second suture is taken between the gastric wall and the second part of the duodenum as near the inner duodenal border as possible, to provide for approximation of 6 to 8 cm of the gastric wall and duodenum (Figure C).
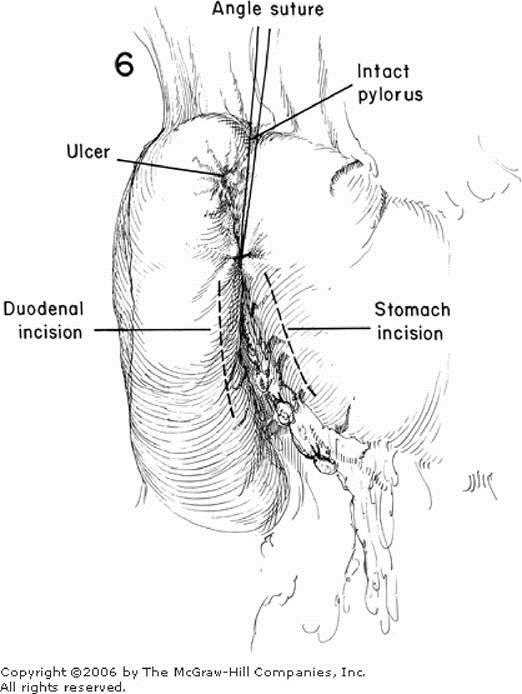
The procedure varies little from that described for pyloroplasty. Sutures of 00 interrupted silk are used on the serosa. Noncrushing clamps should be applied across the gastric wall to avoid gross contamination and at the same time partially control the tendency to bleeding. An incision is made in the gastric wall as well as in the duodenal wall adjacent to the serosal suture line. The pylorus is left intact (Figure 6). All active bleeding points on both the gastric and duodenal sides should be carefully ligated with 0000 silk or similar small-caliber suture material. The mucosa is approximated with either interrupted sutures of 0000 silk or a continuous absorbable suture layer. Interrupted mattress sutures of 00 silk are placed to approximate the seromuscular coat as a second layer (Figure 7). Silver slips may be applied to mark the site of anastomosis. The inferior angle between the second part of the duodenum and greater curvature of the stomach may require several additional interrupted sutures of 00 silk to assure complete sealing of the angle. Either prolonged nasogastric suction should be instituted or a temporary gastrostomy performed (see Gastrostomy), particularly if vagotomy has been carried out.
Copyright ©2006 The McGraw-Hill Companies. All rights reserved. Privacy Notice. Any use is subject to the Terms of Use and Notice. Additional Credits and Copyright Information.