INDICATIONS
Gastrostomy is commonly utilized as a temporary procedure to avoid the discomfort of prolonged nasogastric suction following such major abdominal procedures as vagotomy and subtotal gastrectomy, colectomy, and so forth. This procedure should be considered during abdominal operation in those poor-risk or elderly patients prone to pulmonary difficulties or where postoperative nutritional difficulties are anticipated.
Gastrostomy is considered in the presence of obstruction of the esophagus, but it is most frequently employed as a palliative procedure in nonresectable lesions of the esophagus or as the preliminary step in treating the cause of the obstruction. A permanent type of gastrostomy may be considered for feeding purposes in the presence of almost complete obstruction of the esophagus due to nonresectable malignancy. The type of gastrostomy depends upon whether the opening is to be temporary or permanent.
As a temporary gastrostomy the Witzel or the Stamm procedure is used frequently and is easily performed. A permanent type of gastrostomy, such as the Janeway and its variations, is best adapted to patients in whom it is essential to have an opening into the stomach for a prolonged period of time. Under these circumstances the gastric mucosa must be anchored to the skin to ensure long-term patency of the opening. Futhermore, the construction of a mucosalined tube with valvelike control at the gastric end tends to prevent the regurgitation of the irritating gastric contents.
PREOPERATIVE PREPARATION
If the patient is dehydrated, fluid balance is brought to a satisfactory level by the intravenous administration of 5% dextrose in saline. Since these patients may be malnourished, it is frequently desirable to administer proteins and vitamins parenterally. Whole blood transfusion should be given if there is evidence of secondary anemia or a substantial loss of weight. Intravenous hyperalimentation may be indicated.
No special preparation is required for the temporary gastrostomy, since this is usually performed as a minor part of a primary surgical procedure.
ANESTHESIA
Since some patients requiring a permanent gastrostomy are both anemic and cachectic, local infiltration or field block anesthesia is usually advisable. There is no special indication in anesthesia for a temporary gastrostomy, since this is usually a minor technical procedure that precedes the closure of the wound of a major operation.
POSITION
The patient lies in a comfortable supine position with the feet lower than the head, so that the contracted stomach tends to drop below the costal margin.
OPERATIVE PREPARATION
The skin is prepared in the routine manner.
INCISION AND EXPOSURE
A small incision is made high in the left midrectus region, and the muscle is split with as little injury to the nerve supply as possible, if the gastrostomy is the lone surgical procedure planned (Figure 1). The high position is indicated since the stomach may be contracted and high because of the long-term starvation that the patient may have experienced. The usual temporary tube gastrostomy is brought out through a stab wound some distance from the primary incision and away from the costal margin. The site of the stab wound must correspond exactly to the area of the abdominal wall to which the underlying stomach can be attached without tension (Figure 1).
STAMM GASTROSTOMY
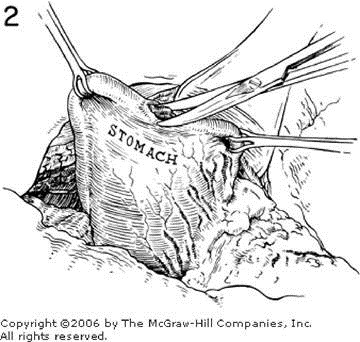
This type of gastrostomy is most commonly utilized as a temporary procedure. The midanterior gastric wall is grasped with Babcock forceps, and the ease with which the gastric wall approximates the overlying peritoneum is tested (Figure 2). An incision at right angles to the long axis of the stomach is made in an effort to minimize the number of arterial bleeders. The incision is made with either scissors or a knife. A mushroom catheter of average size, 16 to 18 French, is introduced into the stomach for a distance of 10 to 15 cm. A Foley-type catheter also may be used. A suture of fine silk may be taken through the entire gastric wall on either side of the tube in order to control any bleeding from the divided gastric wall (Figure 3). When all bleeding has been controlled, the gastric wall about the tube is inverted by the usual purse-string suture of 00 silk (Figure 3). The gastric wall should be inverted about the tube to ensure rapid closure of the gastric opening when the catheter is removed (Figure 6).
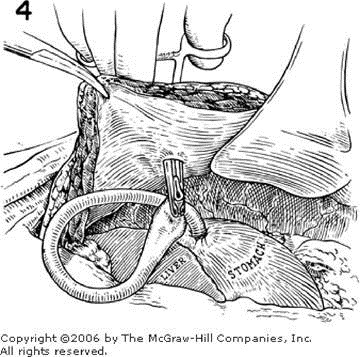
A point is then selected some distance from the margins of the incision for the placement of the stab wound and subsequent passage of the tube through the anterior abdominal wall (Figure 4). The position of the catheter end should be checked to make certain that a sufficient amount extends into the gastric lumen to ensure efficient gastric drainage. The gastric wall is then anchored to the peritoneum about the tube (Figure 5) by four or five 00 silk sutures. Occasionally, additional sutures are necessary. The gastric wall must not be under undue tension at the completion of the procedure. The diagram in Figure 6 shows the inversion of the gastric wall about the tube and the sealing of the gastric wall to the overlying peritoneum. The gastrostomy tube is snugged upward and then secured to the abdominal skin with a nonabsorbable suture.
JANEWAY GASTROSTOMY
This procedure is one of the many types of permanent gastrostomies utilized to avoid an inlying tube and prevent the regurgitation of irritant gastric contents. Such a mucosa-lined tube anchored to the skin tends to remain patent with a minimal tendency toward closure of the mucosal opening.
DETAILS OF PROCEDURE
The operator visualizes the relation of the stomach to the anterior abdominal wall and then with Allis forceps outlines a rectangular flap, the base of which is placed near the greater curvature to ensure adequate blood supply (Figures 7 and 8). Because the flap, when cut, contracts, it is made somewhat larger than would appear to be necessary to avoid subsequent interference with its blood supply when the flap is approximated about the catheter. The gastric wall is divided between Allis clamps near the lesser curvature, and a rectangular flap is developed by extending the incision on either side toward the Allis clamps on the greater curvature. To prevent soiling from the gastric contents and to control bleeding, long, straight enterostomy clamps may be applied to the stomach both above and below the operative site. The flap of gastric wall is pulled downward, and the catheter is placed along the inner surface of the flap (Figure 9). The mucous membrane is closed with a continuous suture or interrupted 0000 silk sutures. The outer layer, which includes the serosa and submucosa, is also closed either with continuous absorbable sutures or, preferably, by a series of interrupted silk sutures (Figures 10 and 11). When this cone-shaped entrance to the stomach has been completed about the catheter, the anterior gastric wall is attached to the peritoneum at the suture line with additional sutures of 00 silk (Figure 12). A gastric tube can be constructed with a stapling instrument.
CLOSURE
After the pouch of gastric wall is lifted to the skin surface, the peritoneum is closed about the catheter. The catheter may be brought out through a small stab wound to the left of the major incision. The layers of the abdominal wall are closed about this, and the mucosa is anchored to the skin with a few sutures (Figure 12). Catheters are anchored to the skin with strips of adhesive tape in addition to a suture that has included a bite in the catheter.
POSTOPERATIVE CARE
When the temporary Stamm type of gastrostomy is used in lieu of prolonged nasogastric suction, the usual principles of gastric decompression and fluid replacement are adhered to. Usually, the tube is clamped off as soon as normal bowel function returns. The temporary gastrostomy provides an invaluable method of fluid and nutritional replacement; compared to the more tedious and less efficient intravenous route, it is the method of choice, especially in the elderly patient.
The temporary gastrostomy should not be removed for at least seven to ten days to ensure adequate peritoneal sealing. In addition, it should not be removed until alimentary function has returned to normal and all postoperative gastric secretory studies have been completed.
When a permanent gastrostomy is done because of esophageal obstruction, liquids such as water and milk may be injected safely into the catheter within 24 hours, while intravenous hyperalimentation continues. Liquids of a high-calorie and high-vitamin value are added gradually. After a week or more the catheter may be removed and cleaned, but it should be replaced immediately because of the tendency toward overly rapid closure of the sinus tract in the Janeway type of gastrostomy.
Copyright ©2006 The McGraw-Hill Companies. All rights reserved. Privacy Notice. Any use is subject to the Terms of Use and Notice. Additional Credits and Copyright Information.